Typhoid fever might be rare in developed countries, but this ancient threat, thought to have been around for millennia, is still very much a danger in our modern world.
According to new research, the bacterium that causes typhoid fever is evolving extensive drug resistance, and it’s rapidly replacing strains that aren’t resistant.
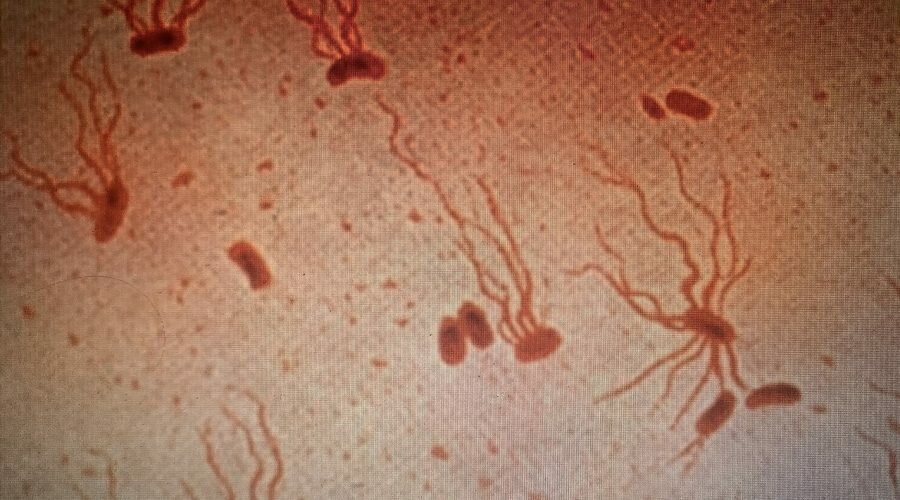
Currently, antibiotics are the only way to effectively treat typhoid, which is caused by the bacterium Salmonella enterica serovar Typhi (S Typhi). Yet over the past three decades, the bacterium’s resistance to oral antibiotics has been growing and spreading.
Sequencing the genomes of 3,489 S Typhi strains contracted from 2014 to 2019 in Nepal, Bangladesh, Pakistan, and India, researchers found a recent rise in extensively drug-resistant (XDR) Typhi.
XDR Typhi is not only impervious to frontline antibiotics, like ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole, but it is also growing resistant to newer antibiotics, like fluoroquinolones and third-generation cephalosporins.
Even worse, these strains are spreading globally at a rapid rate.
While most XDR Typhi cases stem from south Asia, researchers have identified nearly 200 instances of international spread since 1990.
Most strains have been exported to Southeast Asia, as well as East and Southern Africa, but typhoid superbugs have also been found in the United Kingdom, the United States, and Canada.
“The speed at which highly-resistant strains of S. Typhi have emerged and spread in recent years is a real cause for concern, and highlights the need to urgently expand prevention measures, particularly in countries at greatest risk,” says infectious disease specialist Jason Andrews from Stanford University.
Scientists have been warning about drug-resistant typhoid for years now, but the new research is the largest genome analysis on the bacterium to date.
In 2016, the first XDR typhoid strain was identified in Pakistan. By 2019, it had become the dominant genotype in the nation.
Historically, most XDR typhoid strains have been fought with third-generation antimicrobials, like quinolones, cephalosporins, and macrolides.
But by the early 2000s, mutations that confer resistance to quinolones accounted for more than 85 percent of all cases in Bangladesh, India, Pakistan, Nepal, and Singapore. At the same time, cephalosporin resistance was also taking over.
Today, only one oral antibiotic is left: the macrolide, azithromycin. And this medicine might not work for much longer.
The new study found mutations that confer resistance to azithromycin are now also spreading, “threatening the efficacy of all oral antimicrobials for typhoid treatment”. While these mutations have not yet been adopted by XDR S Typhi, if they are, we are in serious trouble.
If untreated, up to 20 percent of typhoid cases can be fatal, and today, there are 11 million cases of typhoid a year.
Future outbreaks can be prevented to some extent with typhoid conjugate vaccines, but if access to these shots is not expanded globally, the world could soon have another health crisis on its hands.
“The recent emergence of XDR and azithromycin-resistant S Typhi creates greater urgency for rapidly expanding prevention measures, including use of typhoid conjugate vaccines in typhoid-endemic countries,” the authors write.
“Such measures are needed in countries where antimicrobial resistance prevalence among S Typhi isolates is currently high, but given the propensity for international spread, should not be restricted to such settings.”
South Asia might be the main hub for typhoid fever, accounting for 70 percent of all cases, but if COVID-19 has taught us anything, it is that disease variants in our modern, globalized world are easily spread.
To prevent that from happening, health experts argue nations must expand access to typhoid vaccines and invest in new antibiotic research. One recent study in India, for instance, estimates that if children are vaccinated against typhoid in urban areas, it could prevent up to 36 percent of typhoid cases and deaths.
Pakistan is currently leading the way on this front. It is the first nation in the world to offer routine immunization for typhoid. Last year, millions of children were administered the vaccine, and health experts argue more nations need to follow suit.
Antibiotic resistance is one of the world’s leading causes of death, claiming the lives of more people than HIV/AIDS or malaria. Where available, vaccines are some of the best tools we have to prevent future catastrophe.
We don’t have time to waste.
Sources:
Publicly released: Wed 22 Jun 2022 at 0830 AEST | 1030 NZST – The bacteria that cause typhoid fever are getting better at evading antibiotics
The international and intercontinental spread and expansion of antimicrobial-resistant Salmonella Typhi: a genomic epidemiology study
Cost effectiveness of typhoid vaccination in India